Resource • Article
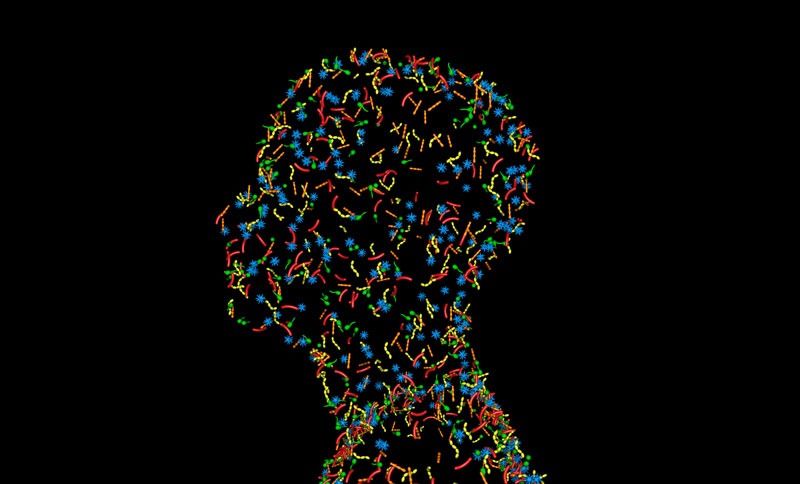
What is the Skin Microbiome?
A current Dove soap ad asks, “Is your body wash microbiome gentle?”
Do you need microbiome gentle soap? And what is your skin microbiome anyway? We’ll answer these questions one at a time.
The microbiome explained
The microbiome refers to the genetic material of all the microbes— bacteria, fungi, viruses and protozoa—that live on and inside the human body. The gut, skin, mouth and vagina all have their own microbial communities that comprise the human microbiome.
According to the Human Microbiome Project, the average human body has ten times more bacteria than human cells. Most of these bacteria work for us rather than against us.
The skin microbiome assists in wound healing, limits allergen and UV radiation exposure, minimizes oxidative damage and helps keep the skin barrier intact and well hydrated. It also fights off threats by external factors such as bacterial transfer from external surfaces, certain cosmetic products, detergents and antimicrobials such as hand sanitizers.
To maintain overall homeostasis, the skin microbiome’s beneficial bacteria have to overpower pathogenic bacteria. When the pathogenic bacteria win out, it influences the skin’s surface and contributes to dermatological conditions such as acne, rosacea, atopic dermatitis, and psoriasis.
Why all the talk about the microbiome?
Using DNA sequencing, researchers are only beginning to uncover links between the microbiome and a host of diseases, including several types of cancer, autoimmune conditions, inflammatory bowel disease, and Crohn’s disease, among others. Generally, microbiomes with less diversity or a lower number of bacteria have a negative effect on human health.
The link between skin microbiome and dermatological conditions
The skin microbiome generally contains four dominant phyla of bacteria: Actinobacteria, Proteobacteria, Firmicutes, and Bacteroidetes. Other, less abundant types of bacteria vary depending on the skin site and the individual. For example, the dry forearm contains mostly proteobacteria, while the glabella (forehead), which is sebaceous (oily), contains primarily Corynebacteriaceae.
Sebaceous areas such as the back, face and behind the ears are typically colonized by Propionibacterium. Researchers have established an association between Propionibacterium acnes (P. acnes) and acne vulgaris. However, P. acnes is also present in healthy individuals. Research suggests different strains of the bacteria may contribute to acne vulgaris.
Bacteria may also contribute to the nonhealing of the chronic wounds. Although bacteria do not cause the initial wound, commensal skin organisms invade and become pathogenic when they breach the skin barrier. These pathogens delay healing and contribute to inflammation.
An rRNA sequencing survey found that bacterial communities colonizing diabetic foot ulcers were associated with certain clinical features. Shallow ulcers, for example, were associated with a greater presence of Staphylococcus spp., while deeper ulcers had greater microbial diversity and a higher proportion of anaerobic bacteria and Gram-negative Proteobacteria.
Treating dermatological conditions through the microbiome
Although topical antibiotics can effectively treat acne vulgaris, they come with side effects and the possibility of antibiotic resistance. Probiotic applications may soon treat acne without disruption to the skin microbiome. Succinic acid, a fatty acid fermentation product of Staphylococcus epidermidis, can inhibit the growth of P. acnes.
As an example of current companies working on this problem, consider AOBiome. They are a clinical-stage microbiome company based in Boston, Massachusetts focusing on restoration of ammonia-oxidizing bacteria to address inflammatory conditions such as acne, allergic rhinitis, migraine, eczema and rosacea. Nitrosumonas eutropha, an ammonia-oxidizing bacteria, generates nitrite and nitric oxide (NO) from ammonia. NO may play a role in wound healing, skin inflammation, and circulation.
But what about my soap?
Cleansers do affect the skin microbiome. However, further research is needed to determine to what extent they impact the body’s largest organ.
A study out of Vienna, Austria, examined the influence of cleansers on infants aged two weeks to 16 months. Researchers found the skin’s pH increased the highest among infants washed with alkaline soap, which has a relatively high pH.
The increase in skin surface pH irritated the protective “acid mantle” and changed the composition of the cutaneous bacterial flora and the activity of enzymes in the upper epidermis. The dissolution of fat from the skin surface may have influenced hydration status, leading to dry skin, the study stated.
Another study looked at how antibacterial soap use impacts the skin microbiome. It found soap use “impacts the community composition of microbes on human skin, but may not affect the taxonomic richness of these communities.”
Addressing FDA’s scrutiny of antibacterial soap ingredients triclosan and triclocarban, the study concluded further research is “especially important in the context of changing lifestyles throughout the developing world, with increases in wealth likely to be associated with increased demand for hygienic products such as antibacterial soaps.” Each year, we discover more about the skin microbiome and its influence on skin health. Advances in DNA extraction and sequencing, combined with software to analyze complex information, will help us get closer to answering the many questions that remain regarding its composition and its role in disease.